Understanding Cancer: What We Know About Lung Cancer
ID
HNFE-981P
EXPERT REVIEWED
Did you know?
Lung cancer starts in the lungs. According to the latest statistics, it was the third most diagnosed cancer and the leading cause of cancer death in the United States (Centers for Disease Control and Prevention, n.d.). Approximately one in 13 men and one in 16 women will be diagnosed with lung cancer during their lifetime (American Cancer Society 2021).
Ninety percent of lung cancer cases are attributable to smoking, making it by far the greatest contributor to lung cancer incidence (American Lung Association 2020). Smoking also increases the risk of death in those who have lung cancer. The risk of dying from lung cancer is 23 times higher among male smokers, and 13 times higher among female smokers, compared to nonsmokers. Other risk factors include exposure to radon and other carcinogens in the workplace and the environment.
The morbidity, mortality, and collective healthcare costs of lung cancer are significant (Sheehan et al. 2019, Agency for Healthcare Research and Quality. 2008). The good news is that lung cancer incidence and mortality rates have been falling over the last two decades as smoking has declined (American Cancer Society 2021). Change in policies and lifestyle behaviors that reduce exposure to agents causing lung cancer will go a long way to eliminating the disease.
Lung Cancer Statistics
(American Cancer Society 2021)
Over the past ten years, the rate of new lung cancer cases has decreased by 23% in men and 13% in women. At the same time, death rates from lung cancer decreased 31% in men and 24% in women.
Estimated number of new cases of lung cancer in 2021:
- U.S. cases: 235,760
- % of all new cancer cases: 12.4%
Estimated number of deaths from lung cancer in 2021:
- U.S. cases: 131,880
- % of all cancer deaths: 21.7%
Five-year Survival Rate
Based on data from the National Cancer Institute Surveillance, Epidemiology, and End Results Program (n.d.), an estimated 22.9% of people with lung cancer will survive the disease five years after diagnosis (fig. 1).
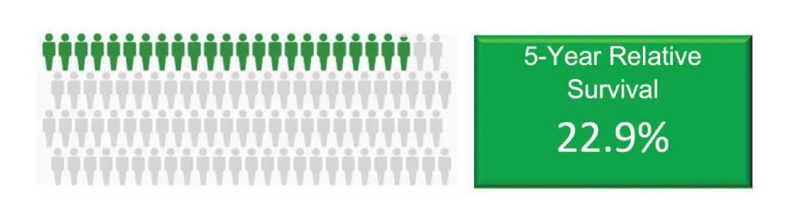
The five-year relative survival rate depends on the type of lung cancer and the stage at which it is diagnosed. When lung cancer is found at an early, or localized, stage, the survival rate increases to 59.8%.
Types of Lung Cancer
(National Cancer Institute, n.d.)
There are two main types of lung cancer. Each grows and spreads in different ways, has different subtypes, and is treated differently.
Non-small cell lung cancer (NSCLC): NSCLC accounts for 85% of lung cancer cases. Different types of NSCLC contain different kinds of cancer cells. Types include squamous cell carcinoma, which forms in the cells lining the inside of the lung; large cell carcinoma, which begins in large cell types in the lung; and adenocarcinoma, which forms in cells that line the lung alveoli.
Small cell lung cancer (SCLC): SCLC accounts for 10%-15% of lung cancer cases. The main types of SCLC are small cell carcinoma, also known as oat cell cancer, and combined small cell carcinoma. These are named for the kinds of cells found in the cancer.
Symptoms of Lung Cancer
(National Comprehensive Cancer Network 2020)
Lung cancer often does not have any symptoms until it has spread. However, some people with early lung cancer do experience symptoms (table 1). Consulting a doctor as soon as symptoms are noticed increases the likelihood that lung cancer will be diagnosed at an early stage. Most of the time, the symptoms will be caused by something other than lung cancer.
| Lung Cancer Symptoms: |
|---|
| Cough that lasts Tiredness that lasts Blood in mucous Pneumonia Shortness of breath Hoarse voice Wheezing Pain on swallowing Pain in chest area Unplanned weight loss |
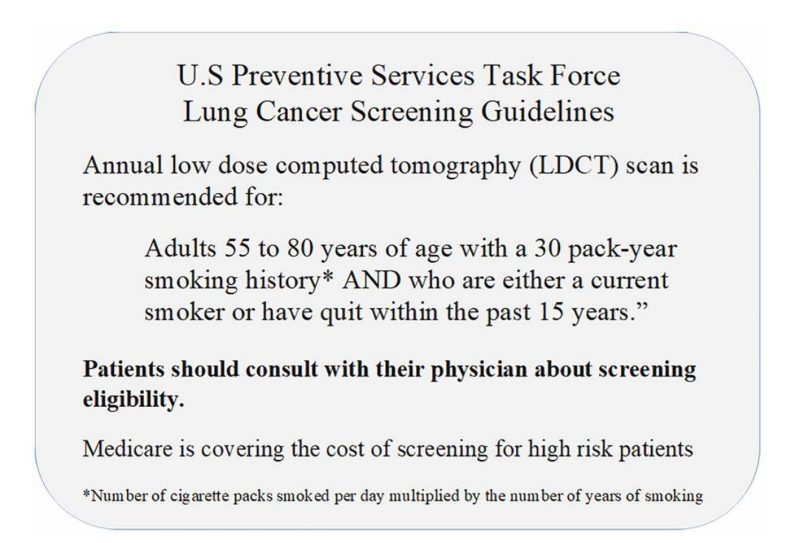
Early Detection and Screening
(U.S. Preventive Services Task Force 2021)
Low-dose computerized tomography (LDCT) has been studied in people at high risk for lung cancer. LDCT uses X-rays to make cross-sectional images of the body. It is more likely than routine chest X-rays to show lung tumors and can show details including tumor size, shape, and position. Because screening with LDCT has been shown to lower the risk of dying from lung cancer, the U.S. Preventive Services Task Force recommends that people at higher risk of developing lung cancer undergo an LDCT scan annually (fig. 2).
Treatment
(American Cancer Society 2021; National Cancer Institute n.d.)
Treatment for lung cancer is specific to the type (NSCLC or SCLC) and stage of the disease. Treatments may consist of surgery, chemotherapy, radiation therapy, targeted therapy, immunotherapy, laser therapy, photodynamic therapy, cryosurgery, electrocautery, or a combination of two or more of these approaches.
Local Treatments
Surgery: Four types of surgery are used to treat lung cancer.
Wedge resection, which removes the tumor and some surrounding tissue.
Lobectomy, which removes a whole section, or lobe, of the lung.
Pneumonectomy, which removes one whole lung.
Sleeve resection, which removes part of the bronchus.
Radiation: Radiation therapy uses high energy rays to destroy cancer cells. There are two types.
External radiation therapy, which uses a machine outside of the body to direct radiation to the area of the body with the cancer.
Internal radiation therapy, which uses radioactive incased substances placed directly into or near the cancer.
Systemic Treatments
Chemotherapy: Anti-cancer drugs are given intravenously, by mouth, or in body fluids or cavities to kill cancer cells or stop them from dividing.
Targeted drug therapy: Anti-cancer drugs travel through the blood to all parts of the body to bring about specific changes in cancer cells.
Immunotherapy: Drugs are used to stimulate a person’s own immune system to recognize and destroy cancer cells more effectively.
Laser therapy: This treatment uses a laser beam to kill cancer cells.
Photodynamic therapy: PDT uses a drug that is activated when exposed to light. The drug is injected and is absorbed in cancer cells. A laser light directed at the cancer cells activates the drug.
Cryosurgery: This treatment uses an instrument to freeze and destroy cancer tissue.
Electrocautery: A probe or needle heated by electric current is used to destroy cancerous tissue.
Risk Factors
Major risk factors for lung cancer include:
- Exposure to tobacco smoke. Smoking or breathing second-hand tobacco smoke is the most significant and preventable contributor to lung cancer. Smoking causes an estimated 90% of lung cancer cases.
- Exposure to radon gas. Radon — a tasteless, colorless, and odorless gas produced by decaying uranium that occurs naturally in soil — is the second leading cause of lung cancer. Homes can be tested for radon, and steps can be taken to reduce concentrations of the gas or remove it.
- Occupational exposure to carcinogens. Toxic substances such as arsenic, chromium, and asbestos — as well as carcinogens found in outdoor air pollution— increase risk for lung cancer.
- A personal or family history of lung cancer.
High Risk Populations
- Populations at particular risk for lung cancer include:
- People over 55 years old.
- Males, especially African American men.
- Those with a history of smoking the equivalent of one pack of 20 cigarettes per day for 30 years or two packs per day for 15 years.
- Those exposed to second-hand smoke.
- Those exposed to other cancer-causing agents, including asbestos, radon, and arsenic.
Prevention
Most lung cancer is preventable. Establishing a healthy lifestyle and avoiding substances known to cause lung cancer are the primary ways to reduce risk.
Don’t Smoke
If you’ve never smoked, don’t start.
Stop Smoking
The risk of dying from lung cancer for someone who has quit smoking is half that of a person who is still smoking (American Cancer Society 2020). There are many resources that can help you to quit smoking.
Avoid Second-hand Smoke
If you live or work with a smoker, urge them to quit or to smoke outside. Avoid areas where people smoke.
Test Your Home for Radon
Have the radon levels in your home checked, especially if you live in an area where radon is known to be a problem. The U.S. Environmental Protection Agency has more information about residential radon exposure in its “Consumer’s Guide to Radon Reduction: How to Fix Your Home” (EPA 2016).
Avoid Carcinogens at Work
Take precautions, such as wearing face masks or gloves, to protect yourself from exposure to toxic chemicals at work.
Eat a Diet Full of Fruits and Vegetables
Choose a healthy diet and consume five servings of a variety of fruits and vegetables daily. Get vitamins and nutrients from food rather than supplements. Avoid large-dose vitamin pills, as they may increase lung cancer risk (Miller et al. 2004).
Be Physically Active
Regular physical activity may reduce lung cancer risk. The Centers for Disease Control and Prevention recommend that adults get two hours and 30 minutes(150 minutes) of moderate-intensity aerobic activity weekly. Examples of aerobic activity include walking, running, swimming, and bicycling (CDC 2020a).
Smoking is the greatest risk factor for lung cancer. The longer a person uses tobacco and the more they use, the greater the risk for developing lung cancer. Quitting smoking before the age of 40 reduces the risk of dying from smoking-related disease by about 90% (CDC 2020b).
Glossary of Terms
alveoli – Tiny air sacs at the end of the bronchioles. The alveoli are where the lungs and the blood exchange oxygen and carbon dioxide during the process of breathing.
bronchus – A large airway that leads from the trachea (windpipe) to a lung.
bronchioles – Tiny branches of the bronchus air tubes in the lungs
five-year relative survival rate – the proportion of persons surviving five or more years after cancer diagnosis compared with the proportion of survivors expected in a set of comparable cancer-free persons.
Additional Resources
National Cancer Institute: https://www.cancer.gov/.
American Cancer Society: https://www.cancer.org/.
Centers for Disease Control and Prevention: https://www.cdc.gov/cancer/.
Surveillance, Epidemiology, and End Results Program: https://seer.cancer.gov/.
National Cancer Institute Surveillance, Epidemiology, and End Results Program – https://seer.cancer.gov/.
American Institute for Cancer Research: https://www.aicr.org/.
Tobacco Cessation Resources –1-800-QUIT-NOW, 1-855-DÉJELO-YA, “How to Quit Smoking” (CDC website with tips from former smokers).
References
Agency for Healthcare Research and Quality. 2008. “Statistical Brief #63: Healthcare Cost and Utilization Project (HCUP).” Modified May 16, 2016. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb63.jsp.
American Cancer Society. 2020. “Health Benefits of Quitting Smoking over Time.” Revised November 10, 2020. https://www.cancer.org/healthy/stay-away-from-tobacco/benefits-of-quitting-smoking-over-time.html.
American Cancer Society. 2021. “Cancer Facts and Figures 2021.”
https://www.cancer.org/research/cancer-facts-statistics/all-cancer-facts-figures/cancer-facts-figures-2021.html.
American Lung Association. 2020. “Lung Cancer Fact Sheet.” https://www.lung.org/lung-health-diseases/lung-disease-lookup/lung-cancer/resource-library/lung-cancer-fact-sheet.
Centers for Disease Control and Prevention. 2020a. “How Much Physical Activity Do Adults Need?” Updated May 27, 2020. https://www.cdc.gov/ physicalactivity/basics/adults/.
Centers for Disease Control and Prevention. 2020b. “Tobacco-Related Mortality.” Updated April 28, 2020. https://www.cdc.gov/tobacco/data_statistics/ fact_sheets/health_effects/tobacco_related_ mortality/index.htm#death.
Centers for Disease Control and Prevention. n.d. “Lung Cancer Statistics.” Reviewed June 8, 2021. https://www.cdc.gov/cancer/lung/statistics/.
Centers for Medicare and Medicaid Services. February 5, 2015. “Screening for Lung Cancer with Low Dose Computed Tomography (LDCT)” (CAG-00439N).
https://www.cms.gov/medicare- coverage-database/view/ncacal-decision-memo.aspx?proposed=N&NCAId=274.
National Comprehensive Cancer Network. 2020. “Guidelines for Patients: Lung Cancer Screening.” https://www.nccn.org/patientresources/patient-resources/guidelines-for-patients/guidelines-for-patients-details?patientGuidelineId=18.
Miller, A. B., H.-P. Altenburg, B. Bueno-de-Mesquita, H. C. Boshuizen, A. Agudo, F. Berrino, I. T. Gram, et al. 2004. “Fruits and Vegetables and Lung Cancer: Findings from the European Prospective Investigation into Cancer and Nutrition.” International Journal of Cancer 108 (2): 269–76. https://doi.org/10.1002/ijc.11559.
National Cancer Institute. n.d. “Lung Cancer–Patient Version.” Accessed May 1, 2022. https://www.cancer.gov/types/lung.
National Cancer Institute Surveillance Epidemiology, and End Results Program. n.d. “Cancer Stat Facts: Lung and Bronchus Cancer.” Accessed May 1, 2022.
https://seer.cancer.gov/statfacts/html/lungb. html.
Sheehan, D. F., S. D. Criss, Y. Chen, A. Eckel, L. Palazzo, A. C. Tramontano, C. Hur, L. E. Cipriano, and C. Y. Kong. 2019. “Lung Cancer Costs by Treatment Strategy and Phase of Care Among Patients Enrolled in Medicare.” Cancer Medicine 8 (1): 94-103.
https://doi.org/10.1002/cam4.1896.
U.S. Environmental Protection Agency (EPA). 2016. “Consumer’s Guide to Radon Reduction: How to Fix Your Home.” https://www.epa.gov/sites/production/files/2016-12/documents/2016_ consumers_guide_to_radon_reduction.pdf.
U.S. Preventive Services Task Force. March 9, 2021. “Final Recommendation Statement, Lung Cancer: Screening." https://www.uspreventiveservicestaskforce.org/uspstf/ recommendation/lung-cancer-screening.
Virginia Cooperative Extension materials are available for public use, reprint, or citation without further permission, provided the use includes credit to the author and to Virginia Cooperative Extension, Virginia Tech, and Virginia State University.
Virginia Cooperative Extension is a partnership of Virginia Tech, Virginia State University, the U.S. Department of Agriculture (USDA), and local governments, and is an equal opportunity employer. For the full non-discrimination statement, please visit ext.vt.edu/accessibility.
Publication Date
July 14, 2022